Most children are accident-prone. They are susceptible to various germs and viruses at school where they slap high-fives and shake hands after sneezing and sit in desks with gum stuck to the edges. They are our little bundles of vulnerable joy. We know we can’t be there to caution their every step, but at the very least, we hope to be able to provide them with health care when they need medical attention.
Medicaid redeterminations are making that difficult. The Division of Medicaid usually redetermines eligibility annually, but the pandemic caused the government to pause redeterminations in March 2020. Three years later, all states were required to resume the eligibility process on April 1. Since then, as the Mississippi Division of Medicaid’s monthly enrollment reports reveal, the department has dropped 18,710 children from Medicaid; more are likely to come.
Many aren’t surprised. The Division of Medicaid has been troubled with inadequate staffing and that will play into their ability to effectively communicate with families known to move frequently. Then there’s the factor that most won’t receive an automatic electronic approval. They’ll have to resubmit or send additional information to prove eligibility, adding another layer of difficulty.
Instead of Saving Money, Save Lives
During the pandemic, Mississippi was not allowed to kick anyone off Medicaid, and because of that, the State received additional federal funds. Instead of letting participants keep access to a full Medicaid plan, the Division of Medicaid secretly put participants who were on a managed care plan—a program for qualifying medical situations that deemed them eligible for a specific period—on a fee-for-service plan to save the agency money.
Instead of paying a managed-care company a monthly rate for each enrollee, the Division of Medicaid only paid providers when the enrollee received care. This private change helped the Division of Medicaid save money. This move was done so quietly that providers didn’t understand why their patients’ coverage had changed with no public explanation. Such underhanded tactics cause people to lose trust in a system that should be helping them whenever they are in need. Help during a unique, worldwide medical crisis should be given generously and not used as an excuse to keep as much money in the government’s pockets as possible.
Many Mississippian postpartum moms and others on the managed-care plan received letters stating their coverage was being canceled. Some received letters later stating coverage would continue, but some didn’t, even though they still had benefits. The lack of information caused countless people not to receive the care they needed because they thought they didn’t have coverage.
People need clarity about their health insurance to make the proper arrangements to avoid losing coverage. That looks different for each participant. It could be backtracking to check mail at previous addresses or trying to contact someone at the Division of Medicaid before benefits are canceled.
For many residents, the damage is done, but moving forward, giving people clarity includes the Division of Medicaid revealing racial and gender data of residents who have lost coverage. We need transparency. The data will provide insight to those that need to be targeted. The Division of Medicaid needs to implement campaigns to increase awareness in these communities and allow people to regain the necessary coverage.
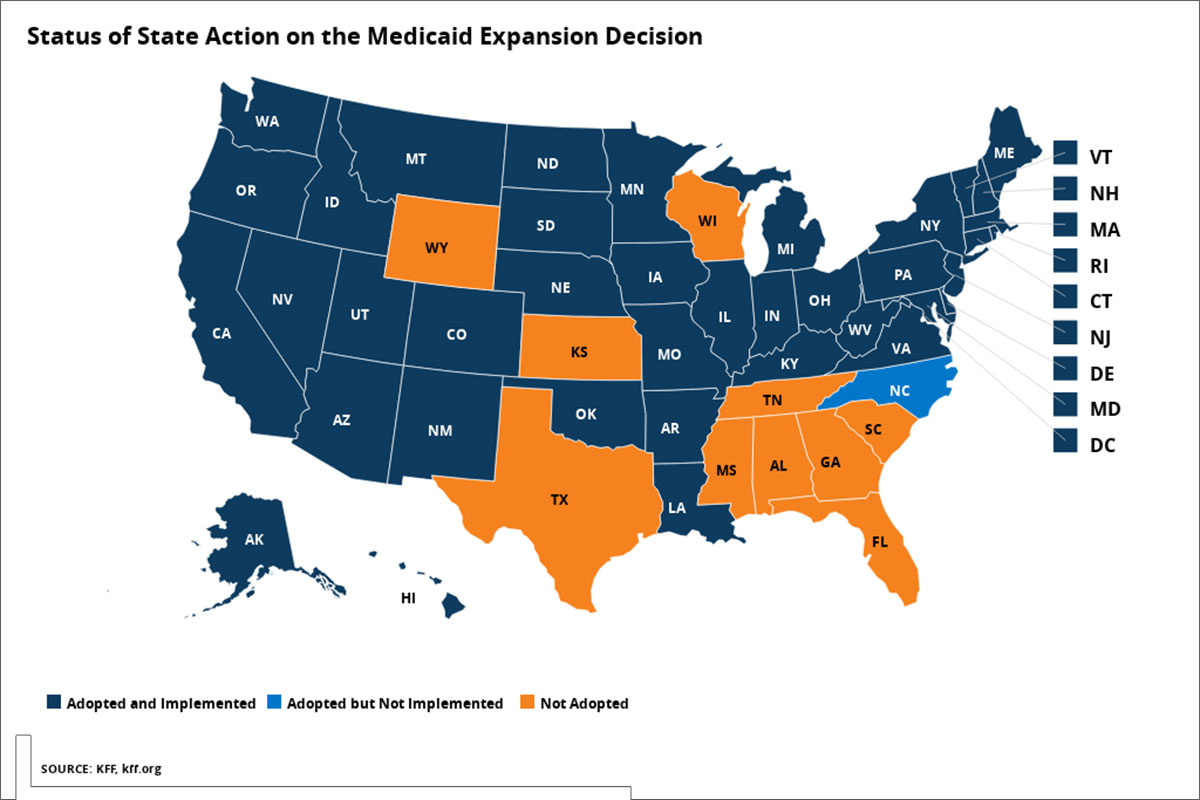
The State should be working to ensure more Mississippians in need have Medicaid, not fewer. Medicaid expansion in a state like Mississippi is a no-brainer. It’s undeniably cruel to refuse to accept federal funds that would provide coverage to hundreds of thousands of working Mississippians who are without health coverage. Clinics and hospitals are closing at rapid rates. People are dying on the side of the road trying to make it to the nearest hospital. Residents are starting to feel hopeless—especially those in marginalized groups.
That hopelessness comes from feeling like politicians don’t care whether they live or die. After all, why wouldn’t the state expand Medicaid? It would bring an estimated $1.5 billion in new revenue annually while creating jobs and helping bolster the budgets of struggling hospitals.
Mississippi, instead of saving money this time, can you save lives?
This MFP Voices essay does not necessarily represent the views of the Mississippi Free Press, its staff or board members. To submit an opinion for the MFP Voices section, send up to 1,200 words and sources fact-checking the included information to azia@mississippifreepress.org. We welcome a wide variety of viewpoints.






