As Mississippi’s looks ahead to the long, difficult task of converting declining transmission of the virus into a final victory over COVID-19, emerging scientific evidence is piling up in support of airborne transmission as a significant—and perhaps primary mode of infection for the virus, experts say.
Mississippi’s recovery has reduced the spread of COVID-19 to a historically low ebb, with Mississippi State Department of Health transmission charts indicating that the state’s new cases have been in freefall since the January peak of the pandemic so far. As of last week, both confirmed cases and confirmed hospitalizations were lower than in early June 2020, before last year’s devastating summer spike.
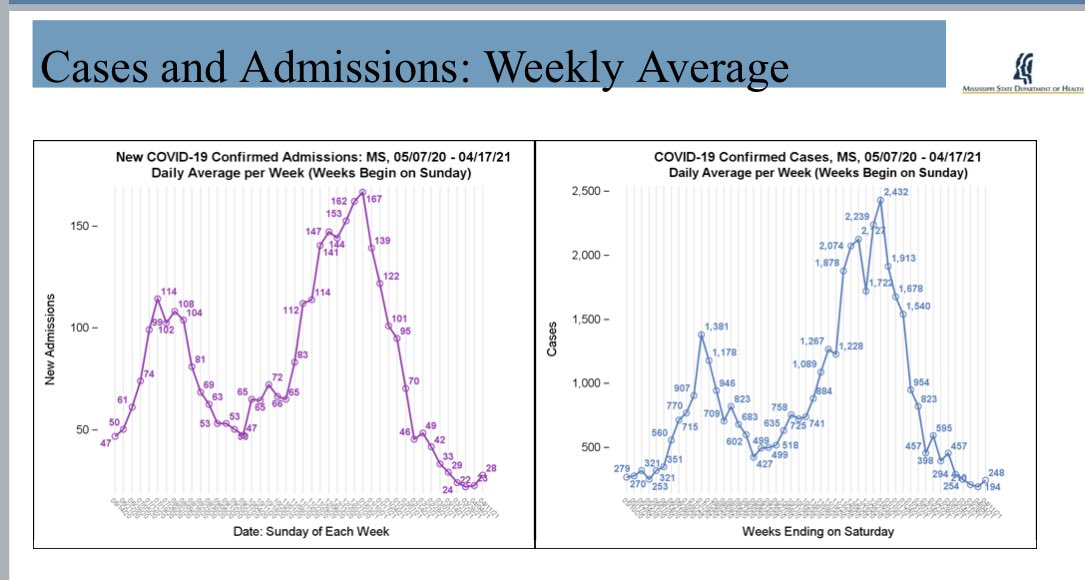
But this number could change. State Health Officer Dr. Thomas Dobbs warned that, for the first time in months, the trough in new cases had shown an incline. “Trending up last week. The future is in our hands. Fight COVID, get vaccinated,” Dobbs said on Twitter.
Vaccinations are in the same position, with MSDH data showing 736,145 fully vaccinated Mississippians so far. But the first concerning trends of a slowdown have begun to emerge, with total vaccinations declining each week in April.
Aerosol Transmission: Primary?
A Lancet study released just last week makes the case that aerosol transmission is the primary mode of infection spreading COVID-19. While expert opinion is that aerosol transmission in some form is a well-established fact, many public-health officials have relegated it to secondary importance behind droplet transmission. The Lancet study provides a comprehensive summary of why the difference between droplets and aerosols matters.
“If an infectious virus spreads predominantly through large respiratory droplets that fall quickly, the key control measures are reducing direct contact, cleaning surfaces, physical barriers, physical distancing, use of masks within droplet distance, respiratory hygiene, and wearing high-grade protection only for so-called aerosol-generating health-care procedures. Such policies need not distinguish between indoors and outdoors,” it reads.
This has been the policy borne out of most U.S. medical expertise for the majority of the pandemic. The relationship between droplet transmission and fomite, or touch transmission, is clear—fear of infected material spread through shared contact with surfaces has driven much of the sanitization and hygiene frenzy of the past year.
Now, while the CDC has acknowledged that the potential for fomite transmission is low, debate over whether droplet or aerosol transmission is the primary mode of infection still rages. If the aerosol method wins out, what might infection control methods look like in the second year of COVID-19?
“If an infectious virus is mainly airborne, an individual could potentially be infected when they inhale aerosols produced when an infected person exhales, speaks, shouts, sings, sneezes, or coughs,” The Lancet article continues. “Reducing airborne transmission of virus requires measures to avoid inhalation of infectious aerosols, including ventilation, air filtration, reducing crowding and time spent indoors, use of masks whenever indoors, attention to mask quality and fit, and higher-grade protection for health-care staff and front-line workers.”
Indeed, overlap exists between these two methods, and responsible reporting on the pandemic has included warnings for both droplet and aerosol transmission. Masks, experts continue to say, are a first-order preventative measure for both droplet and aerosol transmission.
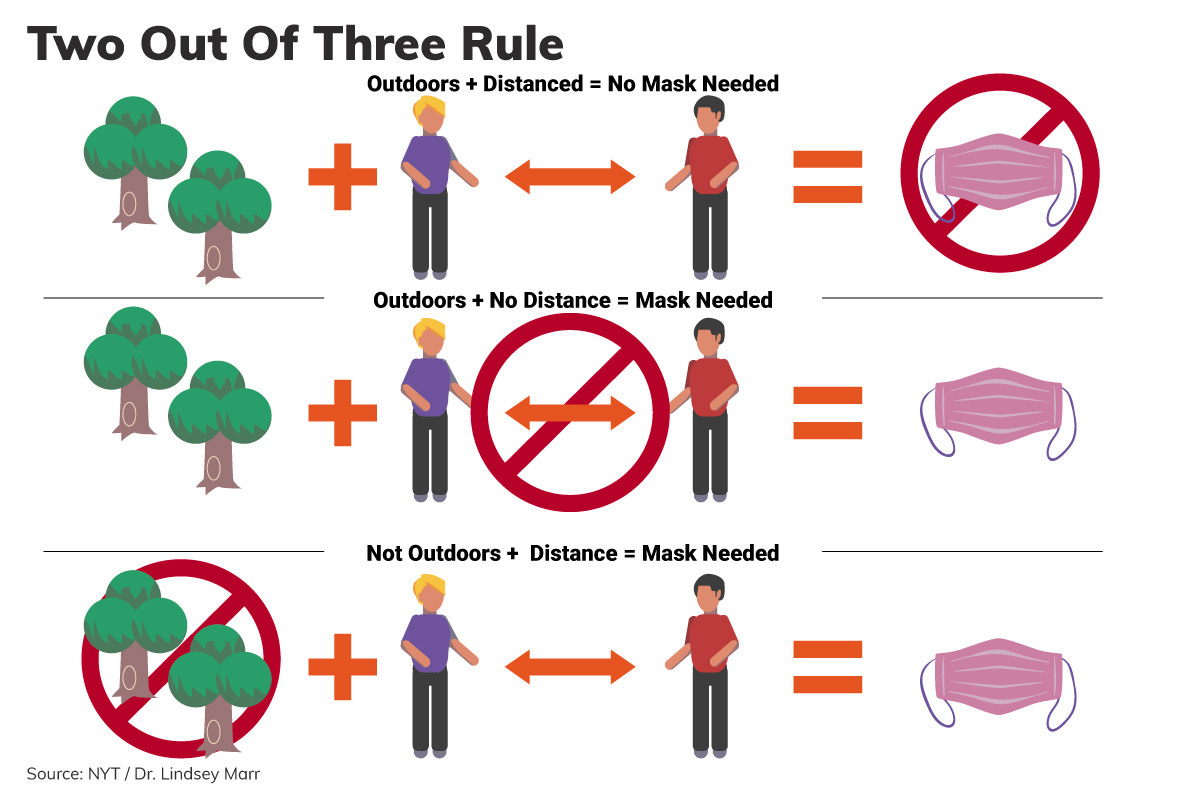
But a focus on aerosols does include a few key differences. Medical officials say ventilation is more critical than distance under such a model—though both matter. Experts say that fully embracing the aerosol model of transmission would allow for moderation of the use of masks outdoors.
Dr. Lindsey Marr, an expert on the subject of viral transmission, told The New York Times this week that she followed the “two out of three” rule for COVID-19 prevention. “If you’re outdoors, you either need to be distanced or masked. If you’re not outdoors, you need to be distanced and masked,” Marr said.
A recent JAMA article provides a more detailed study of how specific building controls can create safer indoor environments, more protected from airborne transmission of COVID-19.
“Controlling concentrations of indoor respiratory aerosols to reduce airborne transmission of infectious agents is critical and can be achieved through source control (masking, physical distancing) and engineering controls (ventilation and filtration),” the authors write.










