A one-year-old in Laurel, Miss., had a blood lead level that was too high, which led Mississippi health officials to visit the city in Jones County in 2015. The child’s blood lead level of 43µg/dL was close to the 45µg/dL level that would have required urgent medical attention.
The unidentified youngster lived in a multi-family rental house constructed in 1950 with a communal kitchen, according to a study the Mississippi Lead Poisoning Prevention and Healthy Homes Program distributed in 2018.
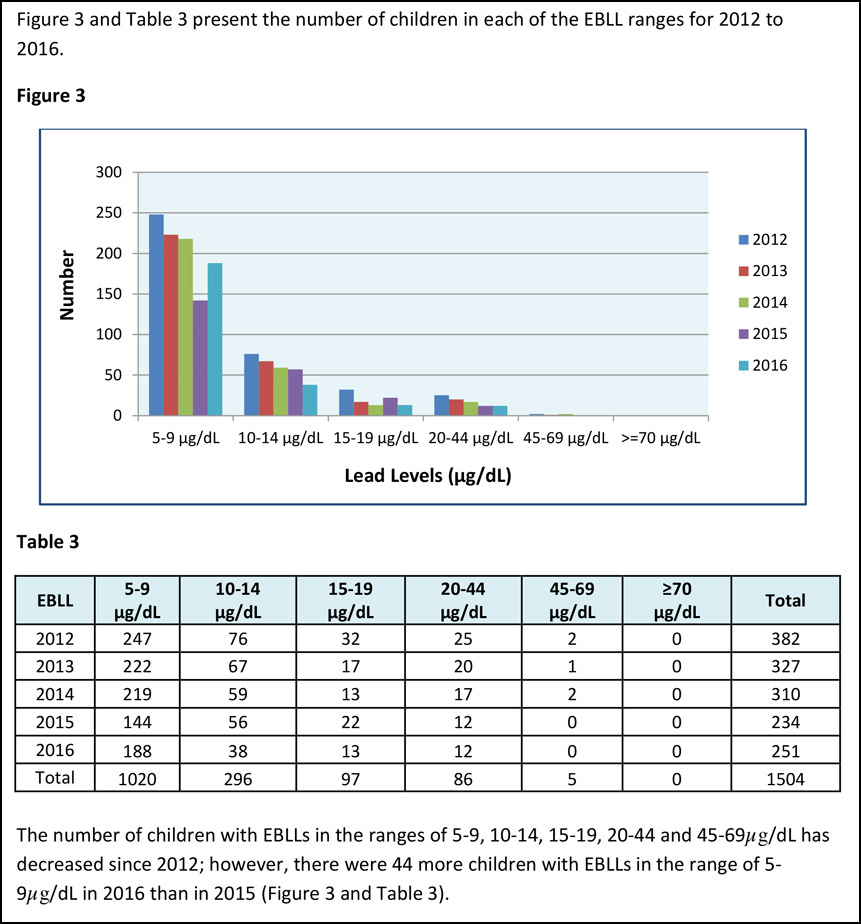
The report, which the Office of Child and Adolescent Health and the Office of Health Data and Research prepared using data from 2012 to 2016 on blood lead testing in children under the age of 6, said lead poisoning is the “number one” preventable environmental health problem for children.
“During the visit (to Laurel), with help from the accompanying translator, program staff was able to identify and test areas where the child had been seen touching or playing,” the report said. “The areas identified with the highest lead concentrations were: the parent’s bedroom, windowsill, the bedroom wood floor, the bathroom wood floor, and the exterior front porch concrete ledge by the main apartment entrance.”
The family should wipe windowsills with soap and water to eliminate lead dust, cover windowsills with contact paper or plastic to prevent kid contact, wet-mop wood floors and use a device like Swiffer instead of dry sweeping, the health officials advised.
“It was subsequently deemed that the home was unsafe and must be vacated,” the report continued.
“This child’s blood lead level has decreased after the home visit, and upon follow-up, after relocation, has continued to go down,” the report added. “On most recent testing, blood lead level had dropped to 13 µg/dL.”
“Recommendations are to continue annual blood lead level screens, monitor developmental growth in the home setting, and continue preventive strategies.”
The report said that the most common highly concentrated source of lead for children in the United States is lead paint.
“When paint containing lead deteriorates into flakes, chips, or fine dust, it is easily inhaled or ingested by small children,” the report added. “The sources of lead exposure continue to be deteriorated lead-based paint and lead dust, but other exposure sources that have been identified consist of vinyl-plastic mini-blinds, job and work-related, home remedies, keys, and Mardi Gras beads.”
Mississippi ranks No. 18 in lead-poisoning cases, University of Mississippi School of Law National Sea Grant Law Center members Stephanie Otts and Catherine Janasie reported in a presentation at the Mississippi Water Resources Conference held in Jackson, Miss., in 2018.
The Mississippi Free Press recently reported that Jackson is facing a major lawsuit over the effects of lead exposure on a group of young plaintiffs.
How Lead Exposure Happens
Lead Free Mississippi coordinator Catherine Lee expressed to the Mississippi Free Press the need for more information about preventing exposure to the metal, citing the fact that there is no known safe level of lead exposure, which has severe consequences for children under age 6. The organization’s mission is to eliminate lead poisoning as a hazard to Mississippi’s children. Lead Free Mississippi is an initiative of Baltimore, Md.-based Green and Healthy Homes Initiative.
Lee said lead poisoning typically affects children under age 6 and pregnant women, and she calls for screening to determine whether a kid is in danger.
“It’s very important that people know the ways in which they could be exposed to lead so we can try to prevent the impacts of lead poisoning, which include lifelong behavioral issues, learning disabilities and the outcomes associated with that,” she said. “I think one of our biggest challenges is to get that information out to medical service providers so they are practicing more of that environmental health education when children are going for regular wellness checks and screenings of other kinds.”
Children are at risk of lead poisoning, the U.S. Department of Housing and Urban Development reports, if they live in a house built before 1950, a house built before 1978 with ongoing or recent renovations or remodeling, or if they have a sibling or playmate who has lead poisoning.
The agency recommends that children’s hands and toys be washed often, that cold water be used for drinking and cooking, and that lead-containing goods be avoided.
Serious Danger in Pre-1955 Houses
Lead paint was used in residential construction from 1884 to 1978 and, prior to 1955, a significant amount of white house paint contained 50% lead in the form of lead carbonate, Dennis Kelly, administrator of the Mississippi Department of Environmental Quality’s lead-based paint program, stated in a webinar held Oct. 27, 2021.

“If I walk past an old house that had white paint on it and I’m brushed up against it, I would get some white powder on my shirt,” Kelly said in the webinar. “That was actually lead oxide from the lead paint oxidizing in the sun. So that’s how prevalent it was—all those white houses.”
He noted that between 83% and 86% of all homes built in the United States before 1978, when the federal government outlawed the use of lead-based paint in residential buildings, still had lead paint, including many homes in Mississippi.
He explained that manufacturers added lead to paint for color and durability in high-traffic areas such as trim around doorways and baseboards, indoor and outdoor wood trim work, and high-gloss surfaces in the kitchen and bathroom. In the factory, they also primed painted metals with red lead (lead tetroxide) to prevent corrosion and rust during transport and storage.
“We’ve had at least a couple of instances where the whole family has been poisoned because dad was working with lead paint or lead-contaminated materials and did not change his clothes before he got in the car and drove home,” Kelly added. “The paint chip, the small size of your small fingernail, is sufficient to poison your typical 12-by-12 bedroom.”
“Lead is extremely sweet. So, therefore (the child) thinks that that windowsill that has lead dust on it is an all-day sucker,” he added. “And we have had several children recently in Mississippi—and by recently, I mean, in the last two years—who had high lead levels because they were sneaking, peeling paint off the wall and eating it.”
“Even children who seem healthy can have high levels of lead in their body.”
Children Absorb Five Times More Lead
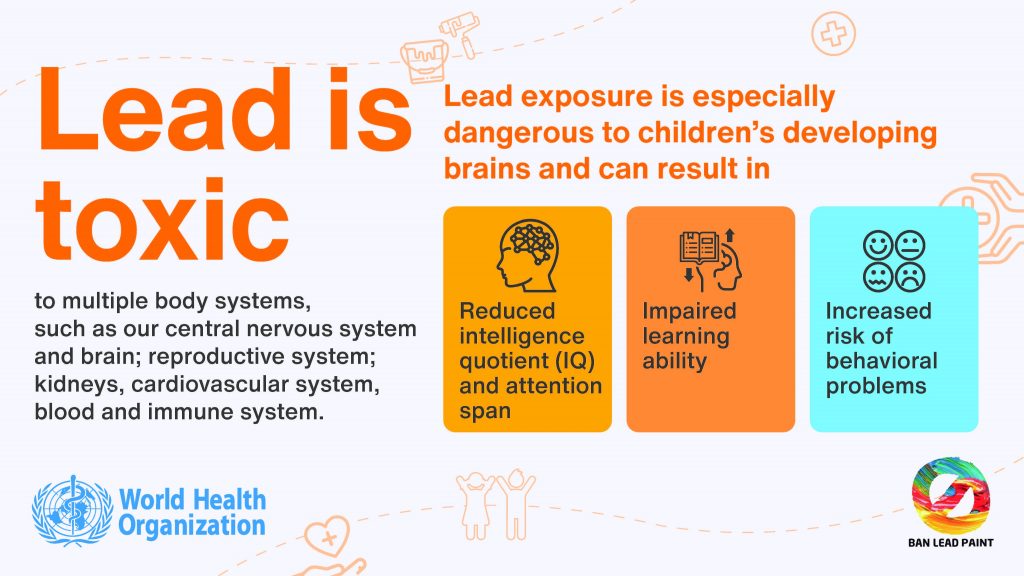
The World Health Organization reports that young children are more susceptible to lead poisoning partly because they absorb four to five times the amount of lead as adults consumed from a given source.
“Lead in the body is distributed to the brain, liver, kidney, and bones,” the organization wrote in October. “It is stored in the teeth and bones, where it accumulates over time.”
“At high levels of exposure (in children) lead attacks the brain and central nervous system, causing coma, convulsions and even death,” WHO added. “Children who survive severe lead poisoning may be left with intellectual disability and behavioural disorders.”
In 2016, Jaime Raymond of the Centers for Disease Control and Prevention wrote that children with high blood lead levels of 70 µg/dL can have serious neurologic abnormalities, including seizures, comas, and even death, and that behavioral disorders are linked to lead exposure even at detectable blood levels of 5 µg/dL or less.

The CDC used to set the blood lead reference value at 10 µg/dL, but reduced it to 5 µg/dL in 2012. The agency announced a further reduction from 5 µg/dL to 3.5 µg/dL in a press statement on Oct. 28, 2021.
“Children of non-Hispanic Black or African American race, those living in low-income households and those who are immigrants or refugees, are more likely to live in communities where lead is pervasive,” the CDC wrote in October. “By updating the BLRV, CDC continues its commitment to health equity by striving to protect children who are at higher risk for exposure to lead.”
Children ingesting contaminated candies and food packaging, soil contaminated by previous sources of lead like vehicle fuel, and activities such as lead mining or smelting pose a danger, the CDC warns.
The organization wrote that the blood lead reference value is to identify children with higher lead levels in their blood compared to most children, based on the 97.5th percentile of the blood lead level distribution in U.S. children ages 1 to 5 years.
Lead-based paints are linked to 80 percent of cases of lead poisoning, Lead Free Mississippi Executive Director Lee said, adding that parents of young infants, particularly those who are bottle-fed, should be aware of the risk of lead in water exposure.
Lee argued for more access to information about lead-poisoning hazards, enhanced blood level tracking and increased investment in lead hazard reduction in households.
“There are new federal funds that are available to do additional lead in healthy homes programs around the state and also (for) more investments into lead (water) service line replacement, (and) the more data that we can get on where the needs are, the more that we could advocate for greater investments in housing and infrastructure,” she added.
New Federal Initiative to Reduce Lead
On Dec. 16, the Biden administration announced renewed funding for various initiatives aimed at reducing lead exposure as a “centerpiece” of the Infrastructure Bill that President Joe Biden signed into law on Nov. 15, 2021.
This includes efforts to replace all lead water pipes within the next decade and funding to replace lead paint in older homes.

“Because of inequitable infrastructure development and disinvestment, low-income communities and communities of color are disproportionately exposed to these risks,” the Biden administration explained.
The Biden administration clarified that $350 million in the American Rescue Plan’s State and Local Fiscal Recovery Fund can be used for lead service-line replacement and lead faucet and fixture replacements. It also announced that the Environmental Protection Agency will allocate $2.9 billion to states for lead service line replacement in 2022, from a total of $15 billion over five years for the Drinking Water State Revolving Fund.
“Non-Hispanic Black people are more than twice as likely as non-Hispanic white people to live in moderately or severely substandard housing, which are more likely to present risks from deteriorating lead-based paint,” the White House said in the press release.

In a book titled “Global Issues: Change and Threat, Geographies of Children and Young People Volume 8,” researchers Bruce London, Cristina Lucier, Anna Rosofsky, and Helen Scharber wrote on the effect of lead and other toxins—Mercury, Carbon disulfide, Manganese, Toluene, arsenic, and Cadmium—on development.
They explained that highly polluted ZIP codes contain more minority and poor residents than other, less proximate ZIP codes. “In other words, the potential health and cognitive implications of exposure to developmental neurotoxicants, especially at a young age, can be seen as a hindrance to social mobility,” they reported.
London, after reading the Mississippi Free Press story on lead in Jackson water, wrote in an email that “My team’s research shows that other developmental neurotoxins also do similar harm to kids’ futures.”
Removing Lead Service Lines
The Natural Resources Defense Council estimates that there are 9.7 million to 12.8 million lead service lines in the country. The Environmental Protection Agency says the figure is between 6 million and 10 million, with “many of them in communities of color and low-income areas.”
The EPA on Dec. 16 announced efforts toward protecting the public from lead in the water, as part of a “whole of government Lead Pipe and Paint Action Plan,” beginning with the establishment of lead service line inventory, a critical step towards realizing the aim of zero lead service line.
In a statement, EPA Administrator Michael S. Regan referenced his recent visits to cities with lead in drinking water.
“Over the past year, I have visited with and heard from communities in Chicago, Flint, Jackson, and many other areas that are impacted by lead in drinking water,” he said. “These conversations have underscored the need to proactively remove lead service lines, especially in low-income communities.”
Kelly, Mississippi’s lead-based paint program administrator, said that lead exposure is generationally dangerous because of storage in the bones during development.
“But what most people don’t realize is that lead exposure as a child is stored in your bones as you’re developing and for pregnant women, if they don’t have a good prenatal diet, then, they will frequently leach lead out of their bones let the fetus get poisoned in the womb.”
In 2011, George Washington University’s School of Public Health and Health Services in Washington, D.C., studied pregnant women, and found the even with lead blood levels well below the reference level, women who had almost any level of lead in the blood had higher blood pressure than their lead-free peers.
Lynn Goldman, then-dean of George Washington University’s School of Public Health and Health Services in Washington, published the study with her colleagues in the Environmental Health Perspectives Journal. “We didn’t expect to see effects at such low levels of lead exposure, but in fact we found a strong effect,” they stated.
They concluded that a significant association between low-level lead exposures and elevations in maternal blood pressure during labor and delivery can be observed at umbilical blood lead levels < 2 μg/dL.
“Because even small reductions in population blood pressure could result in substantial public health benefits, this work suggests that continued reductions in lead exposure remain an important public health goal,” the researchers said.

How Other States Are Reducing Lead
In February 2017, the State of New York awarded $1.5 million to pay for access to tests for lead in their water to anyone in the state.
In 2016, then-Gov. Andrew Cuomo signed legislation requiring immediate testing of drinking water in the state’s pre-1986 school buildings and those that runs on well water every five years. It required that lead levels higher than 15 parts per billion at any tap or faucet with lead levels higher than 15 parts per billion stop being used together with other remediating steps. The government later extended the requirement to all schools.
Maine funds its program to eliminate lead poisoning by charging a fee of 25 cents per gallon of paint sold in the state, establishing the Lead Poisoning Prevention Fund, a 2010 government document said. Its legislature passed a bill to that effect in 2005.
“The establishment of this fund resulted in a significant shift in resources and capabilities for lead poisoning prevention in the state,” the report added.
Green & Healthy Homes Initiative offers a slightly different idea for state and city governments to establish such a fund, to include not just fees, but also fines, and public and private investments, with the funding targeted at providing loans for repair and remediation, to lend to people.

“Key policy actions—removing lead from residential paint, establishing protective drinking water standards, prohibiting use of lead pipes and plumbing, eliminating leaded gasoline, reducing industrial emissions, and shifting to non-soldered food cans—have contributed to a 94% decline in children’s blood lead levels in the U.S. since 1976,” the group said in the proposal. “A focused effort could completely eliminate this problem.”
The organization called for a shift in emphasis from treatment to prevention via necessary investment.
“We spend nearly $300 million a year nationwide to clean up lead and many times more than that to deal with the impact of lead poisoning in children,” it added. “We must invest the amount needed to prevent lead poisoning by removing the risk in the first place, instead of just treating lead poisoning (and paying for it) after it occurs.”
The document cites examples of the fund in three cities—Philadelphia, Pa., Detroit, Mich., and Cleveland, Ohio.
“The Lead Safe Cleveland Coalition is an inclusive public-private partnership founded to address lead poisoning through a comprehensive, preventive, and long-term approach,” a document discussing the establishment of the fund in Cleveland said. “This approach protects Cleveland’s children by merging smart, adaptable public policies; knowledgeable agencies willing to collaborate; proven community programs; and public and private sector accountability.”
Maine’s Lead Poisoning Prevention Fund pays for community and worker-education outreach programs, media campaigns, educational mailings to households with children, an assessment of lead’s current use and the creation of a lead-safe housing registry.
In 2012, Maine added a lead-safe search feature to the state’s housing website, according to the Maine Department of Environmental Protection press release in October that year. “The Maine Department of Environmental Protection’s lead-safety level addition to the site gives renters the ability to find lead-based paint free, safe and maintained property listings,” the press release said.
“The feature will make it easier for Mainers to protect themselves and their families from the harms of lead-based paint, prevalent in properties built before 1978,” it added.
Then-DEP Commissioner Patricia Aho said that the registry recognizes landlords who have taken the right steps to provide healthy housing and helps those committed to keeping their families safe find the information to do so easily.

Texas Program Covers Children 14 and Younger
Texas’ Childhood Lead Poisoning Prevention Program covers children 14 years and younger, whereas Mississippi’s program covers just children 6 years and younger.
The information available at the Mississippi Department of Health website shows that the state’s testing policy is limited to filling out a form at anytime between six months and 6 years of age; at 12 and 24 months, if Medicaid enrolled; between 3 years and 6 years if not tested before that; and annually from six months to 6 years with risk factors. However, in Texas, Parents can ask for testing even without any identified risk.
The National Center for Healthy Housing said that there is need for lead legislation for screening all at-risk children in Mississippi “since presently only Medicaid eligible children are screened, and, of these only approximately 17% of these children are screened.”
MDEQ official Kelly, however, advocated in the October webinar for testing of those who are less than a year old.
“Infants and children under the age of 12 months don’t have any kind of blood testing done for lead unless it’s asked for,” he said. “If you live in a pre-’78 house, especially one that was built before the 1950s, and you have a new baby in the house, that baby should be checked periodically through those early months for lead poisoning, because just a little bit from drinking water, if they switched from a breast milk or formula, they could have a lead exposure.”
“When that child starts getting out of the parent’s arms and down in playpens and walkers and things like that, they really have a major increase in chance of lead exposure, but that testing doesn’t occur until they’re at least 12 months old, and by then damage could really be done.”
“So that’s something to be aware of.”






