The Halleys could not pull their eyes away from the polished doubled doors inside the Jones County Community Hospital that separated them from their son, Jimmy, during one agonizing evening in October 1955. The 15-year-old’s father, Jim Halley, gazed at the barrier and read the bold, golden letters across it: “Polio Isolation—No Admission.”
Much staring and anxiety later, the couple watched as the door finally opened. A man in a white coat strode forward to deliver the verdict.
“The spinal fluid test is positive. Your son has polio,” the doctor told the couple who had traveled an hour southward from their home in Stonewall, Miss., to uncover the cause of their son’s sudden illness.
Before the trip to the Laurel hospital, Jimmy had come home from football practice at Stonewall High School one day feeling ill. He developed a fever, pains in his stomach, dizzy spells, and within a few days, a lurching walk. Schools have often become a vector for outbreaks during deadly epidemics like polio.
As schools prepare to reopen for the 2020-2021 school year in Mississippi amid the current coronavirus pandemic, though, data have shown that, overall, children experience much milder symptoms from COVID-19 infections than adults.
But Douglas Chambers, a historian at the University of Southern Mississippian who has followed COVID-19 data in scholarly fashion since the first case appeared in the state, told the Mississippi Free Press that he fears a little-noticed “pediatric COVID crisis” will overwhelm schools and hospitals this fall—especially if K-12 schools push forward with resuming “traditional” face-to-face classroom settings.
School-age children are now the primary drivers of Mississippi’s increasing COVID-19 caseload, Chambers pointed out.
“And it’s happening the week before schools are supposed to start. It’s a catastrophe,” the scholar said.
Teachers in the state have not shied away from voicing their concerns. One Mississippi school teacher and cancer survivor told the Mississippi Association for Educators in a survey earlier this month that she fears reopenings could jeopardize her life—or that of her 71-year-old mother who lives with her.
“It is too dangerous for both the teachers and the students” to reopen schools, MAE reported one Jackson County educator saying in the survey results it released on July 27. “Teachers should not have to risk their lives to teach.”
An 86% majority of educators statewide told MAE that they had “a negative sentiment about a traditional return to school buildings” for K-12 public schools, and 82% preferred either a hybrid or virtual model over a traditional return. The group released that report even as Mississippi Gov. Tate Reeves has continued to push schools to reopen. COVID-19 cases continue to reach record daily highs in the state, pushing hospitals into crisis mode.
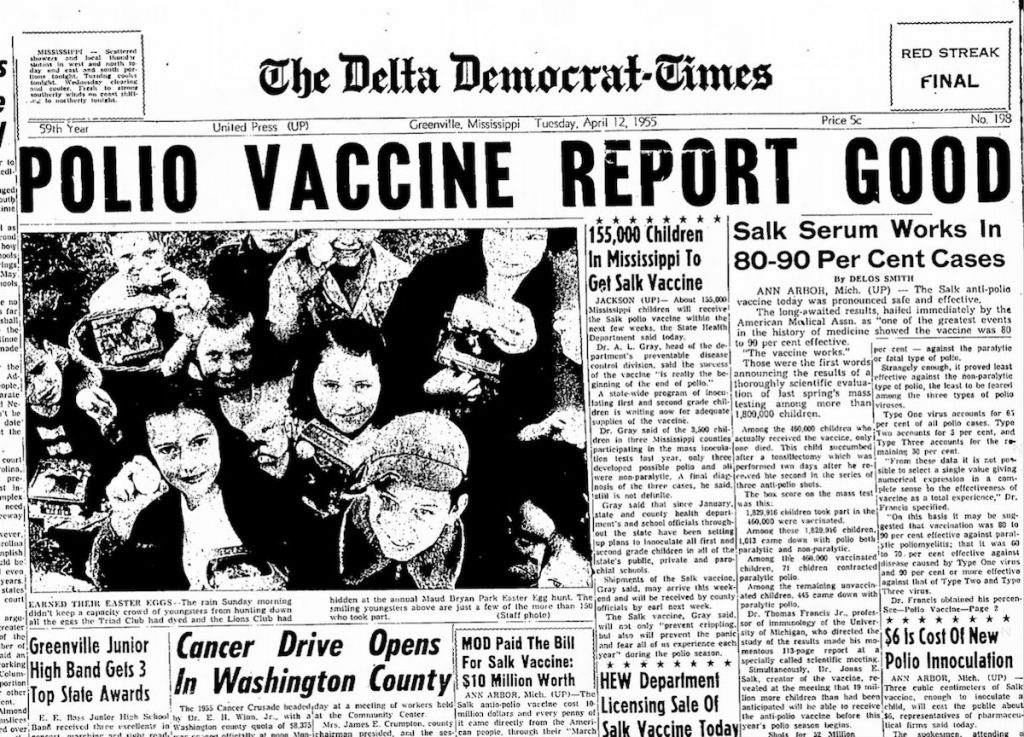
In many ways, the current coronavirus pandemic is different from the polio epidemic that swept the United States from the mid-1940s to the mid-1950s. During much of that era, only the atomic bomb rivaled American parents’ fears. Between 1949 and 1956, around 500 Mississippians contracted polio each year amid a nationwide epidemic, leaving many children dead or suffering from lifelong paralysis.
Since March, the Mississippi State Department of Health has already identified 5,889 pediatric cases of COVID-19—more than the total number of polio cases that physicians diagnosed among all groups in the state during the mid-century pandemic. So far, though, MSDH has only recorded 56 hospitalizations among the state’s novel coronavirus patients who are 17 and younger.
‘It’s a Tidal Wave’
After young Jimmy Halley’s polio diagnosis in 1955, the Halleys did not see their son again for two weeks as he underwent quarantine, evaluation and early treatment, Jim Halley later recounted in a February 1956 piece for his local paper, the Clarke County Tribune. For weeks, they feared that their son might never play football or swim again—or perhaps worse.
He eventually recovered, though, his father wrote. Around the time of the 15-year-old’s illness, vaccines were just arriving that soon eased the fears of polio that had gripped the country for nearly a decade.
The current pandemic, Chambers told the Mississippi Free Press, is “unique.”
“There’s been nothing like this, whether we look at the polio epidemic after World War II, which lasted 10 years, or the 1918 Great Flu pandemic, or in the 19th century, everything from Yellow Fever, to Typhoid, to Cholera, to Smallpox,” the historian said Thursday. “This pandemic is unlike any because, first, like all the rest, COVID-19 spreads exponentially, but unlike the others, it presents incrementally.”
Past pandemics usually hit populations like tall, rogue waves whose terror was quickly recognizable. Bodies littered the streets in Europe during the Bubonic plague in the 1300s, as masses of people all seemed to fall ill at once. And in the 1500s, the Spanish brought European diseases like smallpox and influenza to the Americas, wiping out native populations and bringing the Aztec Empire to ruin in only two years—far more quickly than Spanish Conquistador Hernán Cortés and his armies could have mustered by sheer might.
COVID-19, Chambers said, is a different kind of wave.
“It’s not a big breaking wave. It’s a tidal wave. The water just keeps coming up and up and up. And then it recedes and leaves behind all the mess,” he said, describing devastation similar to that which Hurricane Katrina’s storm surge wrought on the Gulf Coast in 2005.
Instead of mass groups of people falling ill at once, many people who get COVID-19 do not show symptoms for days or even weeks; some never do, but continue to spread the virus in “rising flood”-like fashion. A South Korean study in mid-July found that, while children under age 10 spread the virus less efficiently than adults, those ages 10 to 19 transmit it at about the same rates as adults.
“So my concern is that, because of the way this pandemic works, reopening schools with in-person classes is just going to increase the exponential spread,” Chambers said.
Mississippi set new records on Thursday, as the Department of Health confirmed 1,775 new cases, the most new cases in a single day, and 48 deaths. Hospitalizations also rose to a record 982, even as numerous hospitals across the state have exceeded their capacity for intensive care patients.
Chambers said that, by examining day-over-day increases by age group, the incremental nature of the virus becomes more apparent. On Thursday, the state overall saw a 3.2% increase in novel coronavirus cases. Among 11 to 17 year olds, though, that increase was higher, at 4.1%. The second group with the largest increase came from children ages 1 to 5.
The age group with the third highest increase, though, was among adults ages 30-39. Yesterday’s figures are part of a recent trend, and the rise in infections among 30-somethings, Chambers said, follows an earlier rise among children in recent months.
“Is it any accident that 30-somethings saw a rate increase above the state when it’s tweens and teens and toddlers who saw the greatest increase? These are their parents,” Chambers said. “The narrative has been that it’s the 20-somethings messing this up for everybody, and that’s not exactly true. If it was, we could close down the bars and such. But what can you do if it’s children? They’re not going to the bars. But by next week, they will be going to school.”
Across the state, parents and teachers have voiced concerns that, while most kids may be fine, asymptomatic children will carry the virus to adults who are more vulnerable.
“I think we are rushing it just to make certain people happy,” one unidentified educator told MAE in the July 27 report. “I don’t think we are ready to reopen, and I’m nervous about returning to work. I shouldn’t have to choose between my job and my health.”
Another expressed their worries succinctly: “I am scared to death.”
‘They Will Infect Each Other and Their Families and Their Teachers’
Douglas Chambers first began tracking the coronavirus in March, when MSDH diagnosed the first case in Forrest County, where he teaches at USM in Hattiesburg.
“I have watched this day-by-day go from one person to 57,579 people,” he said Thursday.
In mid-March, Chambers went into a two-week quarantine after developing symptoms that led him to believe he had the coronavirus. The one symptom he did not have, though, was fever, and because testing was sparse at the time, MSDH would not test anyone unless they had a high temperature. The historian put to use the data analysis skills he has refined while studying the transatlantic slave trade over the past 25 years and began studying COVID-19 data.
In the months since, with no classes to teach over the summer, he has written several informal reports and filled a banker’s box with papers from time spent analyzing the pandemic’s spread in 20 U.S. states and 32 countries. He said MSDH’s “transparent, clear and timely” reporting has made it easier to analyze Mississippi’s COVID-19 data compared to other states he’s followed.
“I’m not a doctor. I’m not a pediatrician. But I am a scholar,” Chambers told the Mississippi Free Press. “I’m a professor—a history professor. And we study history for a reason—to see what happened before, to see what people did. And we do that so we can learn from the past. We can learn from that past. And that past can be a week ago, or 100 years ago, or it can be eight weeks ago.”
On Tuesday, the day after MAE released its report, Chambers sent a report to media outlets citing a rising “pediatric COVID crisis” in the state. Children ages 0-17, he reported, are “by far the fastest increasing cohort of new confirmed infections.” Since July 2, he noted, novel coronavirus cases among children more than “doubled to nearly 5,500” (in the three days since his report was released, that number has risen to 5,889).
Earlier this week, Mississippi nabbed the title as the state with the highest percentage of COVID-19 tests coming back positive. All told, about 25% of Mississippians who get tested for the coronavirus are positive, Mississippi State Health Officer Dr. Thomas Dobbs said during a press conference this week. But that figure is even higher among those under 18 years of age, Chambers noted in his July 28 report, citing data showing that 34% of children tested are positive for the virus.
But to get a COVID-19 test, Mississippians must still report symptoms such as fever, chills, cough or runny nose. And since medical professionals nationwide have found that children more frequently carry the virus without displaying symptoms, that means that far more children than detected likely have the virus, Chambers said.
“At this moment, any random 100 children are likely to include at least 10-15, or as many as 30, or as few as 5, depending on where you are, who are largely asymptomatic carriers,” Chambers noted in his report. “They will infect each other, and their families and their teachers. This is the truth.”
The USM professor pointed to the Corinth School District in Alcorn County, which reopened on July 27 and offered parents the choice of either virtual classes or traditional in-class instruction—despite the fact that the county had seen a 10.8% in COVID-19 cases three days earlier, and saw another 9.7% increase on the day the district’s children resumed classes. In the past week alone, confirmed cases in Alcorn County increased by a whopping 39%.
“This is just begging for trouble, and not just for Alcorn County or Northeast Mississippi, but for the state as a whole,” Chambers wrote in Tuesday’s report. “And then very soon, tens of thousands of older siblings will begin returning to college campuses (dorms and dining halls), with classes starting mid-month. This is all very worrisome.”
Chambers’ warning proved prescient. This afternoon, the Corinth School District sent a letter to parents letting them know that it “had a great first week with students back.” In the sentence immediately after that, though, was a less cheerful “COVID-19 Update.”
“We have had an individual test positive at Corinth High School,” the letter read. “Contact tracing at the school has been completed and anyone in close contact (someone who was within 6 feet of an infected person for 15 minutes or more) with this person has been notified. If you were notified, your child will need to quarantine for 14 days from the last known contact. While quarantining, your child may not attend school or any school activities. However, they should continue working digitally in order to be counted present.”
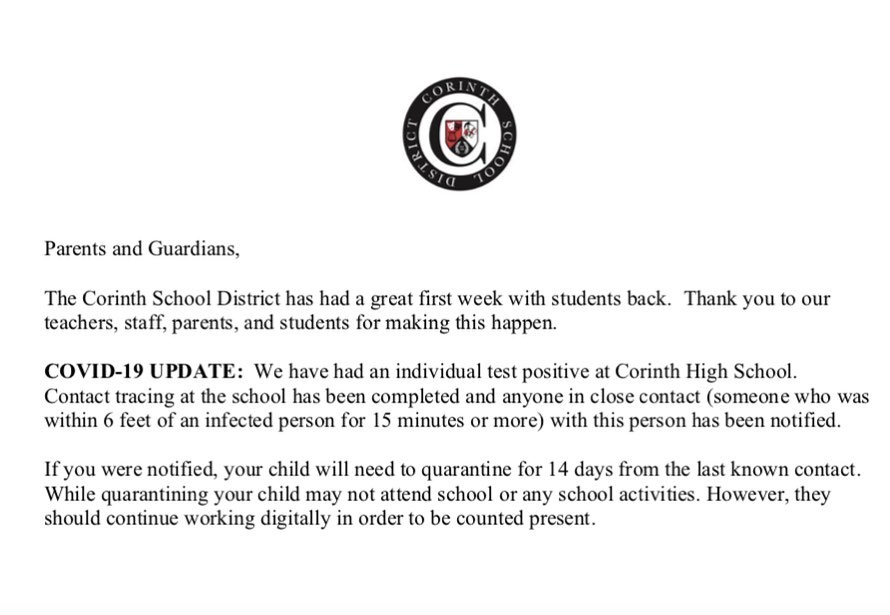
WREG reported that the district is quarantining 12-14 students who were exposed to one infected classmate. Presently, the district is not allowing parents who chose in-class learning to switch their children to virtual classes. Students in grades 4-12 are required to wear face coverings at school, which the district is providing, “unless the class allows for social distancing guidelines,” the district’s reopening policies say.
In the July 27 MAE survey, at least one teacher predicted the scenario that at least a dozen Corinth students are now experiencing.
“Once one person is infected with COVID, that’s a whole class that will need to quarantine for 14 days. We won’t have school anyway,” the educator said. “I think the cycle will repeat itself. So rightfully, the same group of people can possibly be infected twice.”
Other educators voiced both long-standing and new concerns about the state of public education in Mississippi. “Please don’t ask me to spend any more of my own money on supplies. Supply the PPE and the hand sanitizer. Give us our own testing supplies and our own onsite lab,” one teacher said.
“My location doesn’t have a nurse. I would like to see one there,” another said.
A DeSoto County teacher said it would be “impossible” to get necessary safety measures in place by Aug. 6—the day classes are set to resume.
“I beg those who are in decision making positions to please take more time. Death is final and in this case even preventable is schools (implement) virtual or distancing learning for the fall semester as the data is closely monitored,” another said.
One teacher told MAE that she had already had COVID-19.
“I’ve had the virus myself while being pregnant and it was the worst thing I have been through. We need to stop the spread,” she said. “If one teacher gets it, we have exposed almost 100 students plus whoever they came in contact with. Also, with maternity leave, I will use all of my days for that. If I were to get the virus again and have to be out for 14 more days, how would I feed my three kids that month?”
While medical experts say people who have recovered from COVID-19 do have immunity from getting it again in the near-term, it is not yet clear how long that immunity lasts. Experts do not expect a COVID-19 vaccine to become available until sometime early next year at the soonest.
Several educators cited concerns about family members.
“I am very concerned about returning this fall. I have a young child who I have to come home to every day, as well as a mother with an autoimmune disease. My biggest fear is bringing the virus home and possibly giving it to them. … I also think about the students who may be asymptomatic transferring the virus.”
Another cited their spouse.
“I want students to return to a sense of normalcy and stability, which in-person learning would provide, yet I’m also afraid that face-to-face learning will cause a huge uptick in cases,” the educator said. “My husband is high-risk, and I’m afraid of carrying the disease to him.”
‘A Second World State’
Other countries’ experiences with reopening schools amid the pandemic could provide some guidance as Mississippi and other states prepare to reopen schools. Israel resumed schools in mid-May, at a time when the country had brought its daily COVID-19 case increases down from a March 31 high of 738 to fewer than 20 new cases per day.
Within weeks, though, Israel had to begin shuttering dozens of schools, amid severe outbreaks. By the end of June, Israel had wiped out its gains in the fight against the virus and eclipsed its earlier daily highs, and tens of thousands of students and educators had left classrooms to quarantine for two weeks as schools locked down once more. Israel hit a new high on Tuesday, reporting more than 2,000 new cases that day.
“Tracing found that infected teachers who taught multiple classes infected students in each class. As a result, hundreds of teachers and thousands of students were exposed to the virus and spread it to family members at home and beyond, contributing to the resurgence of infections in the general Israeli population,” Israeli newspaper Haaretz reported on July 20.
Mississippi teachers in the MAE survey suggested a different tact, with 40% saying they favored an all-virtual teaching model, while almost 42% preferred a hybrid model, mixing in-class and online instruction.
During the governor’s COVID-19 update press conference on Thursday, Gov. Reeves said he preferred to look at “the numbers” when making decisions about reopening schools. Delaying school reopenings or shifting to online models will deprive schoolchildren who already struggle with learning of much-needed class time, he said. Around two-thirds of Mississippi’s 500,000 children will probably do fine with a virtual classroom model, he said, but for the other third, the detrimental effects of a delayed education could last a lifetime.
“They may never catch up,” he said.
Chambers pushed back on that argument.
“For someone like me, who has been studying this closely day-by-day and watching the virus descend on our children, the governor is doing the wrong math,” he said. “Because children are resilient. Remediation can work. But not if you’re dead, and not if you’re so sick that you can’t study and learn.”
In the July 20 Haaretz report, which offered the U.S. advice on “How to Learn from Israel’s Mistakes,” Allison Kaplan Sommer wrote that school studies were regularly disrupted in Israel over the past two months as schools had to shut down so students could self-isolate for two weeks.
“This is why a binary debate between online learning and returning to in-person is incomplete: It ignores the fact that schools that open are inevitably going to have to periodically pivot back to online tools when they are temporarily closed because of infection,” she wrote.
Sommer cited text messages that Shalva Zalfreind, a 64-year old teacher, sent to parents of her teachers two weeks before she died of a COVID-19 infection earlier this month, begging them to stop sending children to school despite knowing that some members of their immediate family were infected. Older people, the Israeli educator wrote, “do not deserve to die even if they have pre-existing medical conditions.”
In Israel, neither Zalfreind nor other educators were allowed to use sick days to stay out of the classroom; they could either quit or continue teaching. The United States, Haaertz suggested, should take steps to protect older and immunocompromised teachers who are especially vulnerable to the virus.
But unlike Israel, which reopened schools at a time when viral spread was at its low point, Mississippi is set to reopen at the height of the pandemic here so far—and a time when school age children are experiencing high infection rates.
Israel was reporting about two new cases per million people during the week it reopened schools in May. This week, as the first Mississippi K-12 schools opened for the fall in Corinth, the State is daily reporting more than 400 new cases per million people.
Chambers told the Mississippi Free Press that Israel is among the countries he has followed over the past several months as he studied COVID-19 data. Israel is a small country of just under 9 million people—only about three times the size of Mississippi’s population.
“The situation in Israel is comparable, except Israel is a first world country, whereas Mississippi is a second world state,” Chambers said. “For Mississippi, we already have other problems, like underlying poverty, and poverty should be considered an underlying health condition itself.”
Mississippi leaders’ decisions not to expand Medicaid to as many as 300,000 poor families who make too much for traditional Medicaid but not enough for subsidized health plans through the Affordable Care Act makes things even worse, Chambers said.
“The failure of Mississippi to expand Medicaid is now coming back to bite the state in the rear. The failure of Mississippi to properly fund public education, too,” he said. “Now, Israel is an example of reopening schools too early. Israel’s COVID-19 burden was decreasing, and they seemed to have it under control.”
Even before the pandemic, many schools across the state were largely underfunded, especially in the Delta, with critical teacher shortages. Meanwhile, half of Mississippi’s rural hospitals were on the brink of financial collapse. While emergency federal aid has helped some, COVID-19’s mounting toll on hospitals, including from many uninsured people whom hospitals must nevertheless treat, is only adding additional strain. But during his press conference on Thursday, Gov. Reeves reiterated his long-standing opposition to accepting billions in federal dollars to expand the program.
In Chambers’ July 28 report, he cited concerns about another “hidden crisis” within the pediatric one.
“In the absence of either universal or affordable child-care in Mississippi (which is not unique in this respect in 2020 America), and with parents who must work to keep a roof over the family’s head and food on the table, and in time honored fashion among the working poor generally relying on family for basic childcare, my guess is that the older children (teens) and grandparents (50s-60s, even 70s) have shouldered the burden of caring for the younger children,” the historian wrote.
“The risk of intergenerational transmission in this scenario is obvious, both down-age and cross-generational. This is what seems to be happening. This is how pandemics work.”
The teachers, Chambers wrote in his report, “are right,” as is MAE’s report, which said “it has become abundantly clear that we are in no position to proceed as planned.”
“Educators are fearful for our health and the health of our students. We are worried about families and our students’ families,” a July 27 MAE statement announcing the survey’s findings reads. “With the number of COVID cases growing daily, the absence of leadership from our state’s top education officials has been disheartening to say the least.”
With so many children having to stay home while parents “must work to keep a roof over the family’s head and food on the table,” though, Chambers said, it is likely that grandparents will be left caring for children, increasing vulnerability for the age group that is most susceptible to the virus.
‘We Are Struggling to Find Hospital Beds’
Despite lower rates of infection among children, MSDH reports that COVID-19 has hospitalized 55 Mississippi children so far. The state has only one children’s hospital—the Batson Children’s Hospital in Jackson. Among all hospitals in the state capital’s metro area, only four ICU beds remain available, State Epidemiologist Dr. Paul Beyers said in Thursday’s press conference.
University of Mississippi Medical Center Vice Chancellor LouAnn Woodward said last week that “the outlook for hospitals is grim.”
“We are struggling to find hospital beds for all patients who are ill or injured,” she said on July 23.
In his report, Chambers criticized Gov. Reeves for an “upbeat tone” at an earlier press briefing on Tuesday, in which the governor sought to emphasize “the positive.” But “the honest truth is there is very little, if anything, to be optimistic about right now,” the academic said.
“The governor’s sugar-coating (‘finding the positive’) is no help,” Chambers wrote. “He can be honest without being alarmist. But at this point, he cannot be superficially positive without being simply pollyannish.”
On Thursday, though, Gov. Reeves highlighted the dangers of overwhelming hospitals and urged people to “do the little things to help slow the spread.”
“Even if you do not personally fear coronavirus, the overwhelming of our health-care systems will affect everybody. If you get into a car wreck, you don’t want to be treated in a tent like we saw in other parts of the world and, in fact, in other parts of the country,” the governor said.
Still, Reeves did not order a statewide mask mandate. He did order mask mandates in an additional eight counties where outbreaks have been most severe in recent weeks, including: Carroll, Coahoma, Jones, Lee, LeFlore, Lowndes, Noxubee, Pontotoc. But that still leaves 45 of the state’s 82 counties without mask requirements, which Dr. Beyers noted in Thursday’s press conference “prevent transmission significantly.”

Reeves said he has received reopening plans from a majority of school districts across the state, and will “spend a tremendous amount of time this weekend reviewing every one of them” and to offer his thoughts “sometime next week.”
Earlier this week, Reeves said he would not preclude vetoing some local district’s plans for the fall semester if he thinks they endanger the health of students or if he thinks they go too far in stifling their academic achievement. That could include the Jackson Public School District, which announced last week that it plans to go online only for the fall.
The governor’s incremental approach to a virus that “presents incrementally” will not work, though, Chambers said. In his studies of other states and countries, he has found that “what works is bold, decisive intervention, and also whackamoling.”
Reeves’ selective mask orders began in early July with a handful of counties. He has added other counties to the list as increases in COVID-19 cases reached crisis levels in each. That approach, Chambers said, is unwise. He pointed out that every county on the Mississippi Gulf Coast now has a mask mandate except Hancock County, where cases are surging.
“So Bay St. Louis, the party town of Hancock County, people apparently are going there from Harrison and Jackson and Pearl River, and are not wearing masks when they get there because they don’t have to,” Chambers said.
“So here’s my point,” the historian continued. “Failures, half-measures, delays, they’re fatal.”
Chambers pointed to Virginia, his home state, where Gov. Ralph Northam, a physician, implemented a mask mandate in May as he reopened the state’s economy. While cases have increased some there in recent weeks after going down in June, Virginia’s daily raw case numbers remain lower than Mississippi’s, even though Virginia’s population is about three times as large.
‘This is Not Going to Last for 10 Years’
In its July 27 report, MAE recommended that the state should require schools to meet six criteria before resuming in-person classes, including: mandated mask use in all schools; access to “proper training and protective gear,” including face shields “so that students can see non-verbal facial cues”; cleaning supplies and custodial staff to keep all buildings clean and disinfected; training and resources for custodial and other support staff; protocols for checking students’ temperatures when they enter school buildings or board buses; and access to testing for students or educators who show symptoms of the novel coronavirus.
But as children get ready to return to school in the Magnolia State, school districts have not even all agreed to require masks when children return to traditional classroom settings. The Jackson County Public School District on the coast, for instance, decided that masks will be optional for students, teachers and staff when it announced its plans for resuming classes earlier this month.

Chambers said that not only should state leaders like the governor and education officials take the threat of a “pediatric COVID crisis” seriously, but parents should, too.
“If there was a spike among children, it should have peaked and gone down because parents should have freaked out” and nixed playdates and ensured that they and their children masked up before going out, Chambers said.
When his mother was growing up during the polio epidemic, she would always go to her grandmother’s house after school and stay sequestered there rather than spending time with other children afterward, especially around summertime, when polio was most vicious.
During the summer months of the mid-20th century, cinemas, pools and other public facilities where large numbers of people gathered would often close, even though infection rates for polio were far lower than COVID-19.
“That lasted 10 years. And people did it. There was no polio fatigue,” Chambers said.
He noted that, while serious illness rates are currently low among children, two more children were hospitalized from July 27 to July 30. Since the Mississippi Free Press spoke to Chambers yesterday, MSDH confirmed that another child has been hospitalized for the virus.
While Gov. Reeves is spending the weekend reviewing each district’s reopening plans, Gov. Northam has already decided that all public K-12 schools in Virginia will go virtual-only this fall, the historian pointed out.
“Yes, some students will fall further behind. Some children will fall further behind,” he admitted. “But that’s what spring and summer is for. This is not going to last 10 years. It’s going to last another six, eight, maybe nine months. … This idea that there are acceptable levels of risk, or acceptable levels of illness, is just asking for trouble.
“The teachers are deathly scared—and rightly so.”
More information on COVID-19 prevention measures is available at the University of Mississippi Medical center’s website at umc.edu/coronavirus and at cdc.gov/coronavirus.
The Mississippi Free Press has an interactive map showing diagnosed coronavirus cases and confirmed deaths across the state, with county-by-county numbers from the prior day updated each morning.






