Mississippi health insurers will not be required to implement a speedier prior-authorization process nor face fines for any inequalities in provider reimbursement rates after Gov. Tate Reeves vetoed legislation that would have created new regulations on the industry.
“Today, I vetoed two bills that had the potential to seriously increase the cost of healthcare in Mississippi,” the Republican governor tweeted late Wednesday afternoon. “One is a bad idea, and I can’t see myself supporting it. One is a good idea that just includes some correctable mistakes.”
Until Gov. Reeves vetoed it, Senate Bill 2622, known as the Mississippi Prior Authorization Reform Act, would have placed requirements on health-insurance companies to be more transparent about services that require prior authorizations and would have tightened the process for approvals. Health-insurance companies use the prior authorization process to inform providers whether they will cover services, such as drugs or procedures.
“This bill would force insurance companies to give an answer more quickly—great! It also had some unintended consequences,” Reeves wrote Wednesday. “The bill has a lot of technical components: like administrative hearings that are in an incorrect place, untenable costs for Medicaid, and other issues that cause me not to be comfortable signing but hopefully we can get a great bill done soon!”
The bill says it would require a health-insurance company to “maintain a complete list of services for which prior authorizations are required” and to make them “readily accessible and posted on its website”; “prohibit health insurance issuers from denying a claim for failure to obtain prior authorization if the prior authorization was not in effect on the date of services on the claim”; prohibit health insurance companies from revoking or limiting “a previously issued prior authorization while it remains valid”; require insurers to provide information on “how long the prior authorizations for chronic conditions shall be valid”; and mandate that an insurer’s failure to comply with deadlines would “result in any health care services subject to review to be automatically deemed authorized.”
The bill would also have required health insurance companies to set up an electronic portal for prior authorization requests by Jan. 1, 2024, and for providers to use the portal by Jan. 1, 2026. The Mississippi Department of Health would have been authorized to fine insurers that do not comply with its requirements by up to $10,000 per violation.
‘The Insurance Company Won The Game’
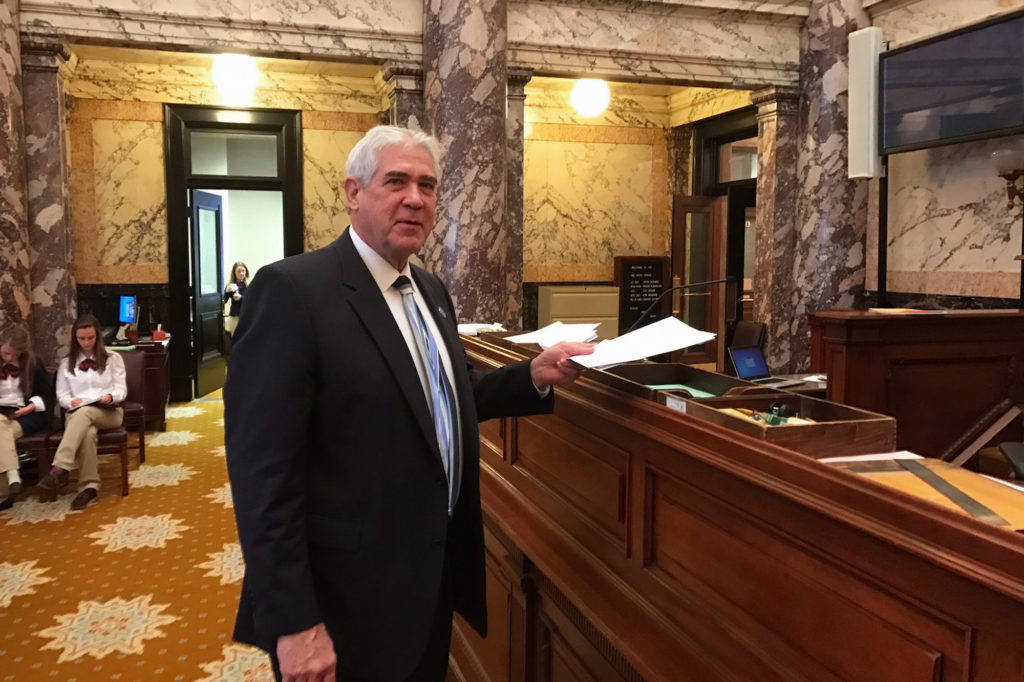
When he introduced S.B. 2622 on the Senate floor in February, Sen. J. Walter Michel, R-Ridgeland, said it was based on “complaints (from) both from doctors and from insurance companies.”
“Doctors said their prior authorization requests weren’t (addressed) timely and they weren’t looked at peer-to-peer. … When they dealt with a prior authorization, they were often dealing with someone clerical or someone who didn’t have that specialty. On the other hand, health insurance companies said, ‘Well, we get accused of being untimely with our prior authorizations but oftentimes doctors are negligent with filling out their forms and don’t get us all the materials we need. So that’s why we’re setting up this portal,” he said.
“It’ll be a real clear issue as to what issues the doctors need to provide to the insurance company so there won’t be this delay. This bill helps both parties.”

In an interview with the Mississippi Free Press Thursday morning, Michel raised concerns about patient care.
“A group of physicians has formed to come together to try to get their needs addressed to where they can get quicker turnaround on getting the care to the patient and not being held up,” he said. “What they have seen in some instances, and it’s really sad, is that if a person is denied, denied, denied long enough, the person will give up on having the procedure performed. In that instance, I guess you could say the insurance company won the game.
“So this would set up a portal on the front end to where the doctor would know (which procedures require prior authorizations). It would not in any way limit an insurance company’s ability to say, ‘This procedure has to have a prior authorization.’ So they could name every procedure out there if they wanted to under the prior authorization list.”
Michel noted that “the more expensive a procedure gets, that’s where the denials are” and said the proposed regulations would “then give us a chance to review it to see what the most commonly denied procedures were.”
In his S.B. 2622 veto message, Reeves said that “almost every Mississippian knows someone who has fought with an insurance company over coverage for a medical procedure or medication that has been recommended for a loved one” and that he supports reforms “to bring transparency, uniformity and timeliness to the prior authorization process.”
Among the reasons the governor gave for vetoing the bill were its requirement for insurers to give a minimum 60-day notice before amending a prior authorization agreement; the fact that it would have granted regulatory authority to the Mississippi Department of Health instead of the Mississippi Department of Insurance; and its requirement for peer-to-peer reviews in the prior authorization process. That requirement would“significantly increase operating costs” that could “be passed on through increased premiums to be borne by Mississippians and Mississippi businesses.”
Michel told the Mississippi Free Press that he believed it was important to keep peer-to-peer requirements in the bill, however.
“What the difficulty has been from what we’ve heard from physicians is that when they’re held up on a procedure, if they think of patient needs, oftentimes they’re dealing with a clerical person at an insurance company or, at the very best, a doctor that doesn’t have the specialty in the issue,” he said. “So we think it’s important that, if an orthopedic doctor is going to be recommending a ACL surgery or a or knee replacement, that if (a patient) is denied the procedure, that he or she should be able to talk to an orthopedic who is representing the insurance company, not an ear, nose and throat doctor. So we thought that it was very important to have the peer-to-peer review in the bill.”
He said Reeves’ concerns about which department has authority to enforce the bill, however, was not a “sticking point” with him. “It would be fine with me if the insurance commissioner would like to oversee the program,” he said.
Before the veto, S.B. 2622 earned unanimous approval in the Mississippi Senate and passed the House 108-5.
‘It’s Not What You Expect In Mississippi’
The bill Gov. Reeves called a “bad idea” is Senate Bill 2224, which would allow the Mississippi insurance commissioner to “adopt rules and regulations to examine and address any inequalities or irregularities regarding provider reimbursement rates paid by an insurer, subcontractor, third-party administrator or other payor regarding covered services received by covered persons in this state.” The regulations would “allow an insurer to show evidence as to why any inequality or irregularity may be justified” with fines up to $10,000 per violation.
On the Senate floor in February, the bill’s sponsor, Sen. Kevin Blackwell, R-Southaven, said Mississippi’s Republican insurance commissioner, Mike Chaney, requested the legislation.
S.B. 2224 comes on the heels of last year’s contract dispute between Blue Cross Blue Shield, the state’s largest insurer, and the University of Mississippi Medical Center, the state’s largest hospital. UMMC leaders accused the insurer of reimbursing the hospital at lower rates compared to other academic medical centers in nearby states, and patients lost care for eight months before the insurer and hospital reached an agreement.
The bill earned unanimous approval in both the Mississippi House and Senate. But on Wednesday, Reeves made clear he will not support it in any form.
“They can massively fine private insurance if they aren’t ‘equittable’ [sic] enough” under Blackwell’s bill, Reeves tweeted. “That is crazy. It’s not what you expect in MS, but that’s why we read every bill closely!” (The bill does not, however, refer to “equity,” which is not the same as “equality.”)
In his S.B. 2224 veto message, Reeves criticized what he called “an accelerated attempt” over the last decade “to erode the free market in exchange for bureaucratic control over all aspects of our lives” and claimed it would negatively affect Medicare and Medicaid plans.
“It is typically justified by our country’s political power structure, and their commitment to ‘equity’ at any cost. We are typically asked to hand power to a small cadre of government officials in order to achieve equity, and they are given unprecedented power to pursue this goal,” the veto message says. “… Such power would bestow on the Commissioner the unchecked authority to review the reimbursement rates set by contract between healthcare providers and third-party mayors and arbitrarily mandate that a higher rate be paid under the threat of a $10,000 penalty for each service provided at a perceived inequitable rate.
“In short, SB 2224 would empower the Commissioner to invalidate the terms of contracts between private parties and make the Commissioner the rate czar for healthcare in Mississippi,” it continues. “The grant of such authority would … result in an increase in already too-high insurance premiums paid by hardworking Mississippians and Mississippi businesses who are participants in the private insurance market.”
The Mississippi Free Press asked Blackwell for comment on Reeves’ veto this morning. “I’ve got no comment right now on it,” the Republican senator said.
Veto Overrides Possible
After the Mississippi Free Press asked his department for comment this morning, Mississippi Insurance Commissioner Chaney, a Republican, said in a statement this afternoon that he was “certainly disappointed in the Governor’s veto message for SB 2224 and SB 2622.”
“Both of these bills are consumer-friendly bills that would benefit healthcare providers and consumers in our state. The Governor is sadly mistaken that SB 2224 would have affected Medicare and Medicaid plans as the Department of Insurance does not have jurisdiction over these plans and the bill did not expand that jurisdiction,” Chaney said. “Senate Bill 2224 would give the Department of Insurance the important tools necessary to ensure that Mississippians would continue to have access to quality healthcare at reasonable rates.”

The Legislature could still override Reeves’ veto of either bill with a two-thirds vote from both houses during the next legislative session in 2024.
Sen. Michel, who is the chairman of the Senate Insurance Committee and the author of S.B. 2622, told the Mississippi Free Press on Thursday morning that a veto override is possible.
“It all depends on what the lieutenant governor wishes to do, whether he wishes to override the veto,” he said. “I’ve already had several senators come up to me and tell me they really thought it was a good bill, and they would be with me if we decided to do an override. So, I believe it will be very easy for every senator to go back to their district and say, ‘We passed a bill that’s good for our doctors, is good for our patients, it’s good for health care.”
In his message Wednesday, Reeves said he was “reviewing every bill” closely and had examined 76 bills this week with only two vetoes.
“Good folks can sometimes let bad things past the goalie, and we’re the last stop before disastrous consequences like massively increased healthcare costs,” the governor wrote. “Glad to do it!”
‘He Wouldn’t Let Us Address This Issue’
In an interview after this story first published, Chaney said that, after reading Reeves’ veto messages, he doesn’t “know what the hell he’s talking about” and implied the governor may be trying to help insurance companies. He also criticized Reeves’ remarks about “equity.”
“That’s rhetoric to try to paint somebody as ‘woke.’ … That’s rhetoric for the crowd,” the Republican commissioner said, explaining that the inequalities he hoped S.B. 2224 would address include cases in which health insurance companies reimburse Mississippi providers for significantly less than they reimburse providers for the same services in other states. But that could also include inequalities in reimbursements within the state, too, he added, such as in the majority-Black Mississippi Delta region.
“I don’t call the governor a racist, but there’s been some irregularities in reimbursement for Delta hospitals versus metro area hospitals,” Chaney said.
The commissioner disagreed with Reeves’ claims that the bills would increase health-care costs and predicted they would result in lower costs even as providers received higher reimbursements. Chaney said Reeves previously blocked similar reforms from becoming law when he was lieutenant governor, and estimated that the failure to change how care is reimbursed “has shortchanged health care providers in this state since by $150 million to $200 million a year.”
“When he was lieutenant governor, he wouldn’t let us address this issue. Anything we tried to do on regulatory examinations was blocked,” said the commissioner, who added that he has not spoken with Reeves this year.
In Reeves’ veto message for S.B. 2224, he wrote that while “one insurance commissioner may apply such a tool conservatively and restrain himself from playing kingmaker, another may be far less just.”
During the interview, Chaney mused about the difficulties of passing insurance reimbursement reforms when “a lunatic governor” is in office. “I’m not calling the current governor a lunatic, but a future governor may be a lunatic,” he added.
If the Legislature does not override the governor’s veto next year, Chaney said, he will likely “wash his hands and move on.”
“I’m not trying to pick a fight,” he said. “I’m just trying to keep consumers from getting screwed in this state.”
This story has been edited to remove a repeated quote.










