The COVID-19 pandemic highlighted how seriously individuals with cardiovascular disease and related comorbidities should consider their overall health and wellness. Risk factors including obesity, high blood pressure and high LDL cholesterol (or bad cholesterol) proved to worsen outcomes for patients who contracted the coronavirus.
Cardiovascular disease is already the leading cause of death in the Magnolia State. Nearly one-third of Mississippians live with high cholesterol. So why aren’t more therapeutics accessible for those who wish to manage these risk factors and keep them under control?
The Partnership to Advance Cardiovascular Health recently released an alarming report citing that insurance companies were more likely to deny life-saving medications to lower harmful cholesterol levels for women, Black and Hispanic patients than male and white patients. Mississippi ranks among the highest states in claim denials. Blue Cross Blue Shield Mississippi has a 49% rejection rate for these medications.
Some people can alter their diet and increase their exercise routine to make their LDL levels manageable. Still, others with pre-existing conditions and hereditary high cholesterol need medication to lower their levels. Now more than ever, patients need access to medications that can reduce cholesterol up to 70% and cut the risk of a heart attack up to approximately one-third.
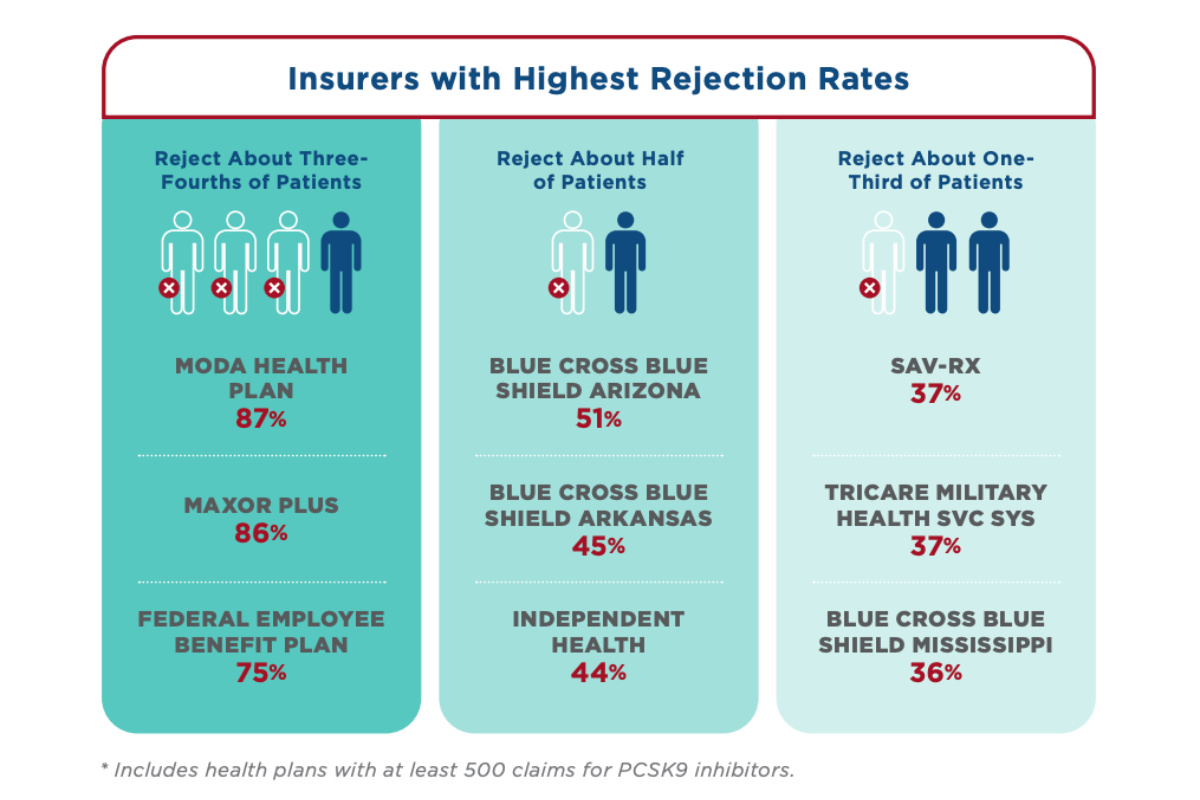
The compounding effects regarding the prevalence of high cholesterol within Black communities and higher-than-average prescription coverage denial rates in Mississippi are troubling. We must improve preventive care if we want better patient outcomes surrounding cardiovascular disease.
Mississippians have three ways to address lowering LDL levels in our state.
Screenings, Education and Prescription Access
Most people with high cholesterol show no signs or symptoms. However, a simple blood test can measure your cholesterol levels. Your health-care provider can do this in their office, which is often a covered benefit through many insurance plans. If you do not have a primary-care physician, check your local health clinics for availability or free screening events in your local community. Many churches and nonprofit organizations provide cholesterol screenings for the community free of charge at various points in time.
If someone in your family has high cholesterol or takes medicine to control cholesterol, you will need to monitor your cholesterol levels more actively. Once patients know their cholesterol levels, they have the power to change the dire outcomes that may arise from untreated high cholesterol. An open dialogue with your clinician will help them decide which treatments are best for you. Many options are widely available to manage high-cholesterol levels easily, but you must start somewhere.
The best way to avoid high cholesterol that is not hereditary is to eat healthily and incorporate more physical activity into your life. Assess your risk factors. For example, you are more likely to have high cholesterol if you are overweight, if you smoke or if you struggle with diabetes. Learn to avoid foods high in saturated fat and start small with physical activity, like walking around the block a couple of times a day. Small changes can make significant improvements to your health.

Understanding your target levels is essential to knowing whether you are on the right track. Everyone is different, so your target cholesterol levels may be slightly lower or higher depending on your age, sex and heart-disease risks.
Working with a dietician can help you better understand healthy swaps you can make in the kitchen to improve your cholesterol levels. Food is a big part of our culture and can be a means of bringing the family together. Plenty of recipes, however, do not require ingredients that significantly raise your cholesterol, so you need not sacrifice flavor when cooking or avoid family gatherings because you fear that the prepared dishes may affect your heart health.
If you are a smoker, now is the time to quit. People who smoke cigarettes tend to have high total cholesterol. This is not an easy effort, but many insurers offer smoking-cessation programs tailored to your needs to better your chances of success. It is never too late to quit smoking; the sooner you do, your body can begin healing.
We have seen great advancements in innovative medications to help patients with cardiovascular-related diseases, but they only work if patients can afford and access them. Physicians often prescribe advanced therapies like PCSK9 inhibitors to patients who struggle with managing their cholesterol levels or who have genetic conditions that increase their risk of high cholesterol to help lower their LDL levels.
Insurers need to provide open access to these advanced therapies and remove barriers like prior authorizations that get in the way of patients receiving these life-saving treatments.
If your pharmacist has ever told you that they are waiting for the insurance company to approve your medication, this is prior authorization. These tactics delay and sometimes prohibit access to life-saving medicines. Removing prior authorizations or at least extending the approval period could help all Mississippians who need access to cholesterol-lowering medications.
We cannot make a measurable difference in cardiovascular outcomes unless we all—patients, providers, health systems and insurance companies alike—find solutions to overcome barriers that unnecessarily delay access to care. We need our communities to lean into preventive care; we need our physicians to screen and treat; and we need our insurers to eliminate unnecessary barriers to care. A healthier Mississippi starts with tackling cardiovascular disease head-on.
This MFP Voices essay does not necessarily represent the views of the Mississippi Free Press, its staff or board members. To submit an essay for the MFP Voices section, send up to 1,200 words and sources fact-checking the included information to azia@mississippifreepress.org. We welcome a wide variety of viewpoints.